Diabetes Management
Diabetes and Diabetic Retinopathy
With diabetes mellitus, your body cannot use and store sugar properly. Increased blood sugar levels can damage blood vessels in the retina, in the back part of the eye. This is referred to as diabetic retinopathy.
Types of Diabetic Retinopathy
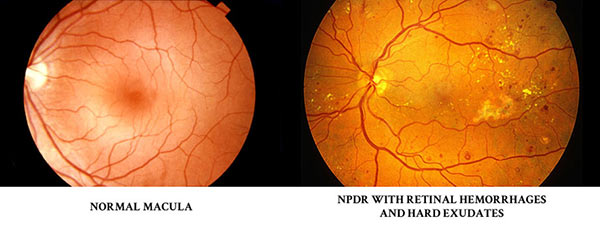
Nonproliferative (NPDR) or background diabetic retinopathy is the an early stage of diabetic retinopathy. This stage causes tiny blood vessels in the retina to leak blood or fluid. The fluid causes the retina to swell or form deposits called exudates. Most diabetics have mild NPDR and it usually does not affect their vision. The longer that you have diabetes and/or the more poorly your diabetes is controlled, the more likely you are to have some form of diabetic retinopathy.
Diabetic Macular Edema The leaky blood vessels in the retina can cause swelling in the central part of the retina, called the macula. This can significantly affect a person’s ability to see. Diabetic macular edema can be successfully treated with intravitreal injections and possible laser to prevent further vision loss.
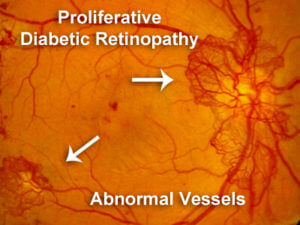
Proliferative diabetic retinopathy (PDR) is where abnormal new vessels (neovascularization) grow on the surface of the retina or optic nerve. These new abnormal vessels are weak and tend to break or rupture causing blood to fill the vitreous (a vitreous hemorrhage.) There is also a risk of retinal detachments and other retinal disorders. PDR may also cause neovascular glaucoma, where new abnormal blood vessels grow onto the iris (the colored part of the eye) clogging the drainage channels of the eye and causing dangerously increased eye pressure. This elevated pressure (neovascular glaucoma) can rapidly cause damage to the optic nerve resulting in permanent blindness very quickly.








